Published in Healthcare Manager, Autumn 2019. Photo: Stefano Pollio/Unsplash
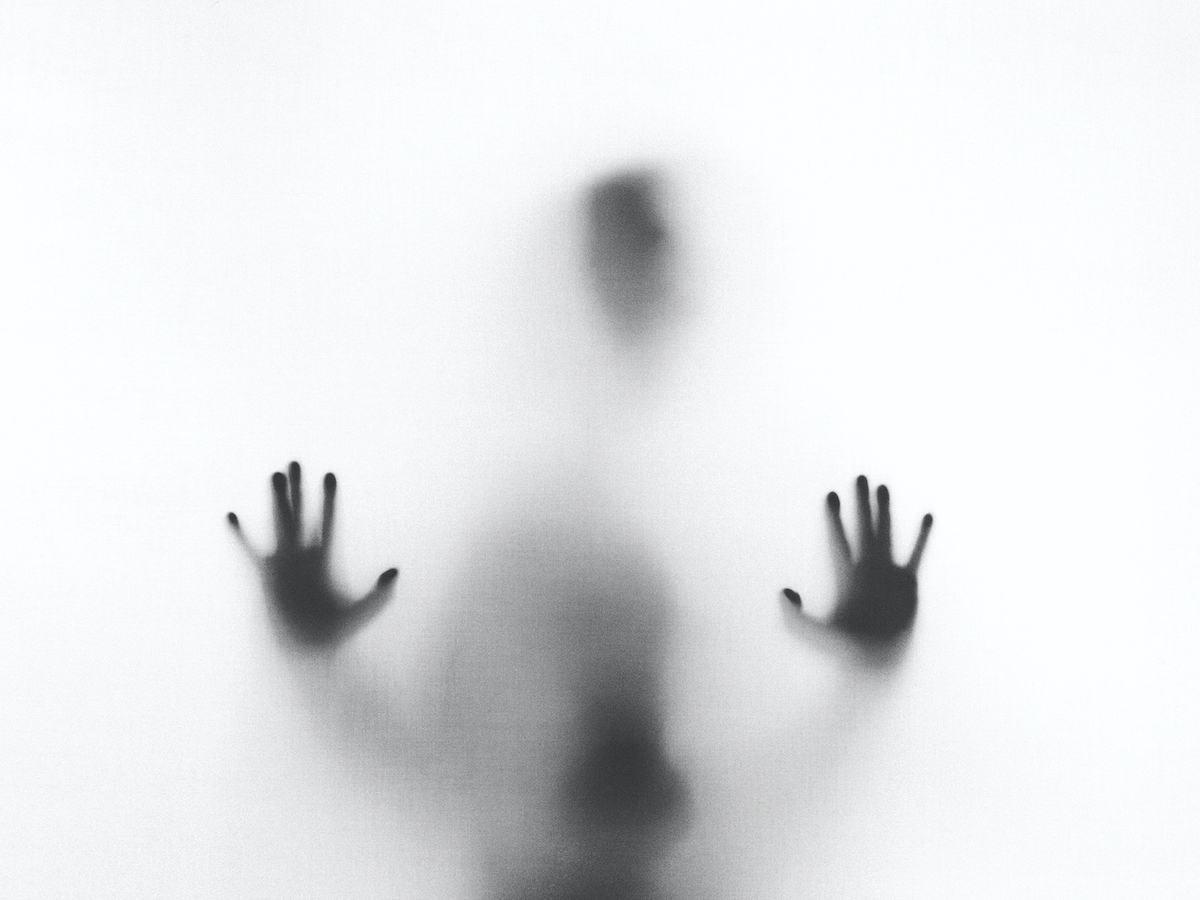
SPECIAL REPORT: In a disturbing new trend, a small but growing number of NHS managers are being diagnosed with workplace PTSD. Craig Ryan spoke to three MiP members who have paid a high price for the NHS’s failure to tackle toxic workplace bullying.
After months of bullying and extreme pressure at work, and following another traumatic meeting with her boss, Laurie, a senior manager with an NHS system body, broke down on her way home. “It was Christmas and I remember seeing the lights in the city centre,” she recalls. “I was crying and crying on the train and I tried to read a book so people couldn’t see how much I was crying. I don’t remember walking home at all.”
Laurie was soon suffering from suicidal thoughts and “horrible dreams” in which senior managers were trying to hang her. Her GP and a psychiatrist eventually diagnosed her with Post Traumatic Stress Disorder (PTSD), and she is now on a waiting list for therapy.
“Getting up for work would be almost impossible at the moment, so it’s really limited my life,” she explains. “I take anti-anxiety medication and anti-depressants, and I’m under a psychiatrist as well. The anti-anxiety tablets have calmed me down an awful lot, otherwise I wouldn’t even be able to have this conversation.”
Laurie believes her condition may be related to an extremely traumatic experience during her teenage years, which she disclosed to her occupational health department. Although they agreed with her PTSD diagnosis, Laurie’s employer provided no support and did nothing to tackle the bullying that brought it on.
“Almost anything stresses me now. I clam up and freeze very easily,” she explains. “PTSD strips away trust and it becomes scary—I mean, imagine not being able to trust your own family. And dealing with a lack of trust is emotionally, and therefore physically, very tiring.”
Many readers will be horrified—even incredulous—that PTSD, a condition associated with military veterans, victims of natural disasters and witnesses to horrific events, has become an occupational hazard in the NHS. Can you really get shell shock, as PTSD used to be known, just by doing your job as a healthcare manager?
Sadly, yes. Although PTSD is traditionally defined as originating in a single traumatic event, mental health practitioners in Europe and America now recognise that the same symptoms can result from continuous exposure to very stressful situations, such as serious bullying and verbal, emotional or sexual abuse. The term ‘Complex PTSD’ (cPTSD) is increasingly used to describe this condition, and is recognised as a variant of PTSD by the support charity PTSD UK.
The symptoms of cPTSD and conventional PTSD are identical: flashbacks, nightmares, panic attacks, high anxiety, severe depression and suicidal thoughts—often accompanied by alcoholism or drug abuse. Both are psychiatric injuries which can be treated and are not related to personality disorders.
Workplace PTSD (or cPTSD) is caused by prolonged exposure to extremely stressful situations such as bullying, abuse or harassment. Common factors in the cases known to MiP include:
- Serious bullying by a manager or series of managers, extending over months or years, and often including gaslighting or mobbing
- Inexplicable and sometimes bizarre behaviour by managers, which is tolerated or even encouraged within the organisation
- Employers ignoring occupational health reports and independent medical diagnoses
- Individuals being kept in the dark about allegations against them
- Lack of support following previous traumatic experiences at work
- Victimisation and blaming managers for issues outside their control
- Treating mental illness as a performance management issue or character flaw
- HR and senior management backing the bully rather than the victim
MiP is aware of about a dozen members who have been diagnosed with workplace-induced PTSD. Most of them are women, reflecting the well-established finding that PTSD is more likely to affect women than men. Laurie is one of three women who agreed to share their experiences with Healthcare Manager on condition of strict anonymity. They have all been fully supported by MiP but, to protect their identities, we cannot reveal details of the support they received.
Like many PTSD sufferers, senior nurse manager Giselle began to drink more heavily to numb her symptoms as they developed. Her doctors believe she contracted PTSD as a result of her employer failing to deal with the psychological impact of a serious patient safety incident many years earlier, and subsequent blatant bullying from a series of managers. Giselle’s condition became so severe, she was only stopped from taking her own life by police intervention.
“The PTSD diagnosis was suggested by the [cognitive behavioural] therapist and my GP, and a psychologist confirmed it,” Giselle explains. “Three times I’ve had trauma at work and then I go into this cycle of mental health deterioration… and then in the end it becomes a disaster, and I reach a crisis point.
Rather than accept responsibility, Giselle’s employer used her symptoms against her and ignored advice from occupational health. “The trust completely said this was about my behaviour; that it’s not about mental health, it’s a character flaw,” she says.
MiP national officer Ruth Smith, who has dealt with a number of workplace PTSD cases, says employers have been slow to recognise the condition and rarely offer the right support. “Even when they acknowledge that someone is suffering from a mental health condition, there’s an expectation it will be a ‘normal’ condition like anxiety or depression,” she explains. “The fact is that counselling and occupational health support just isn’t enough to shift PTSD.”
In rare cases where PTSD-specific therapies—such as eye-movement desensitising reprocessing (EMDR)—have been tried, they’ve met with “considerable success,” she adds.
Ruth believes the PTSD cases known to MiP represent the thin end of the wedge. “What happened to many of these women—being bullied out of the job—is actually very common now, but we can’t often report it because people just leave and sign non-disclosure agreements,” she says. “These people have reacted psychologically very badly to something that is going on quite widely. Other people might suffer from stress and anxiety instead.”
She stresses that employers have a responsibility to take action and cannot just expect people to cope. “Too often, employers are not willing to make the reasonable adjustments needed for people with serious psychiatric injuries to return to work,” she warns. “That just puts pressure on people who are already vulnerable. Some of our members have suffered one breakdown after another because their employer has failed to take action despite knowing that they have a serious mental illness.”
Clinical manager Steph has undergone bullying and gaslighting behaviour from a senior colleague for more than 12 years. This includes spreading and encouraging false rumours about her, deliberately exaggerating problems and even making a false and malicious complaint to Steph’s professional regulator.
“She flatly just lies—that’s her usual way of operating,” says Steph. “But even when you know she’s lying, it does make you doubt yourself… I did get my line manager and a board member involved, but nobody did anything about it—they were all just pussy-footing around her.
“She was furious that I’d been to [the board member] and she came over to the office and was screaming in my face,” Steph adds. “I thought she was going to hit me.”
Steph also experienced group bullying or ’mobbing’ at the hands of other colleagues, many of whom seemed to have been intimidated by the same manager. “I ended up in a situation where this really close clique of people were judging my every word and move,” she recalls. “It was like they were saying, ‘you’re nothing here, this is our world’. I heard them talking about other people in the same way. It was like a gang culture—an all for one and one for all kind of thing.”
Even after occupational health had accepted she was suffering from a mental health condition as a result of previous traumatic experiences at work, Giselle was repeatedly bullied by her then chief executive, and later by her line manager, a member of the trust board.
“I started to get micromanaged, I started to get bullied, I started to get humiliated,” she recalls. Like Steph, she feels other colleagues were intimidated into joining in. “It was almost like classic childhood bullying. You’re being bullied at school, so you become unpopular and everyone just migrates over there because it’s safer. People were thinking, ‘If it can happen to Giselle, it can happen to anyone’.”
She found occupational health (OH)sympathetic but ultimately powerless. ”The therapists they referred me to suggested PTSD, but the trust wouldn’t engage,” says Giselle. “We asked them why they didn’t use the OH report but they just said, ‘We didn’t think it was relevant’. I mean, how could it not be relevant?… I was made to feel like I was lying, that I was making it up about having mental health issues to cover up my alcoholism.”
No one involved with Giselle’s investigation had any knowledge of mental health issues. “One HR manager admitted that he’d made up his own diagnosis about me, even though he wasn’t qualified to make a diagnosis about anything,” she recalls.
Laurie had a similar experience. “OH recognised my condition and recommended a stress risk assessment,” she explains. “At a meeting, my manager actually had the report in his hand, but just ignored it and carried on… repeating all these allegations for which he had no evidence whatsoever.”
As she describes it, Laurie’s ordeal resembles a Kafkaesque nightmare, in which she was kept in the dark about allegations against her and left in state of confusion by her employer’s increasingly bizarre behaviour.
“They kept sending me letters that conflicted with each other,” she recalls. “One letter would conflict with the last letter, or the letter would conflict with itself, and still there was no information about what I’d done wrong, so I was utterly confused by it all.
“I thought at some point they were going to stop because it was just crazy, but it felt like they’d let it get so out of control they didn’t have a way out of it themselves. I had a schedule of allegations which my MiP rep said didn’t amount to anything—they either had no evidence or were really minor. One them was a complaint that I’d opened a window at a meeting!”
MiP’s Ruth Smith says bizarre behaviour by employers is a common feature of the most serious bullying cases. She describes one case in which a member was inexplicably threatened with performance management measures shortly after returning from maternity leave.
“It was a high-performing service which fell apart when our member was away, because managers refused to backfill her post,” Ruth explains. “They had nine months of disaster, but within a few weeks they were putting pressure on her, asking why the department hadn’t come back into line.
“Managers suddenly started questioning whether she was too young to be in a senior post and making sexist comments about her appearance,” Ruth continues. “Our member was never told what she’d done wrong, and just couldn’t understand why this was happening to her. They were desperately trying to make out it was an issue with her performance, when there’d never been one previously.”
These three cases fit a disturbing pattern MiP has observed in dozens of bullying cases across the NHS: evidence from the employee, their GP, therapists and even the organisation’s own occupational health services is ignored, while unsubstantiated allegations, trivial complaints and even rumours are taken seriously and used as the basis for aggressive disciplinary or capability action.
“When someone has suffered a psychiatric injury at work, it’s often a result of the way they’ve been treated by the management team,” explains Ruth. “And then we get this defensiveness on the part of the organisation. They close ranks and go to great lengths to protect the bully. And we know that this person will do it again. It’s about power. The bully is often someone who everyone is afraid to stand up against.”
Employers often seem to get locked into a cycle of defending the indefensible for fear of incurring legal liabilities, she adds. “It becomes easier to just dismiss the person who’s being bullied than to continue having them in the workplace. The amount of public money that goes on all the processes, disciplining people and fighting cases, is ridiculous.”
The real tragedy is that the serious mental illness inflicted on these women—and the other members MiP has supported—were not just the result of the inevitable pressures of working for the NHS. They were caused by the failure of particular employers to tackle bullying at work, or to take seriously the mental health problems it can cause. For that to happen in the NHS—which more than any other employer ought to understand mental health—is a nothing short of a national disgrace.
- The names of the MiP members participating in this story have been changed to protect their identity. To read more about MiP’s campaign against bullying in the NHS, visit the MiP website.